Influence of climate change on legionellosis and minimizing the health consequences of Legionella
In the period from August to September 2023, 166 people in Poland were infected with Legionella of which 23 died. The water supply system of the city of Rzeszów was found to be contaminated with the bacteria [1]. There was another outbreak in Wuppertal in August of the same year. Thirteen cases of illness caused by Legionella were reported. The city suspects that the cause of the outbreak was a cooling or air conditioning system that had encouraged the spread of the bacteria [2]. In 2023, Germany reported an increased number of Legionnaires’ disease cases observed in the ambulatory/occupational setting. In the 33rd week, 99 infected persons were recorded [3]. The rising summer temperatures due to climate change have an impact on the number of cases of infections caused by Legionella pneumophila. The increased humidity and precipitation are associated with a higher incidence of Legionnaires’ disease. In addition, climate change influences the base temperature of household water pipes. The cold water temperature is increased due to the rise in air and soil temperature, which allows better bacterium growth [4].
Pathogen and occurrence
Legionella pneumophila is an aerobic, gram-negative, motile, non-spore-forming rod bacterium. They belong to the genus Legionella which comprises around 40 species with over 60 serogroups. In principle, all Legionella are classified as potentially pathogenic to humans. Legionella pneumophila is the most relevant species for humans (approx. 90%). The bacterium causes Legionnaires’ disease and Pontiac fever. Approximately 75% of infections are community-acquired and are caused by the pathogen L. pneumophila serogroup 1.
Legionella bacteria are widespread environmental germs. They are found in soils, water accumulations, drinking water systems, recooling plants, and sewage treatment plants. Optimal growth takes place at temperatures between 25 °C and 45 °C. Above 60 °C the germs die. There is a regular increase in legionellosis in the summer and autumn months due to higher temperatures and possible stagnation in the water pipes, which favors biofilm formation and therefore optimal growth of the pathogens [5].
Legionella: Route of infection, incubation, and symptoms
The main route of infection is through the inhalation of aerosols containing Legionella. Another, rarer possibility is the aspiration of contaminated water. Direct human-to-human contagiousness has not been proven. The incubation period for Legionnaires’ disease (with pneumonia) is approx. 2-10 days, usually 5-6 days. In the case of Pontiac fever (without pneumonia) it is approx. 5-72 hours. The most common symptoms in those affected are flu-like symptoms, headaches and aching limbs, severe pneumonia, and diarrhea or vomiting. The high-risk group for the disease caused by L. pneumophila consists of people with impaired immune defenses, people with lung diseases, and smokers [5].
Legionella: Diagnostic
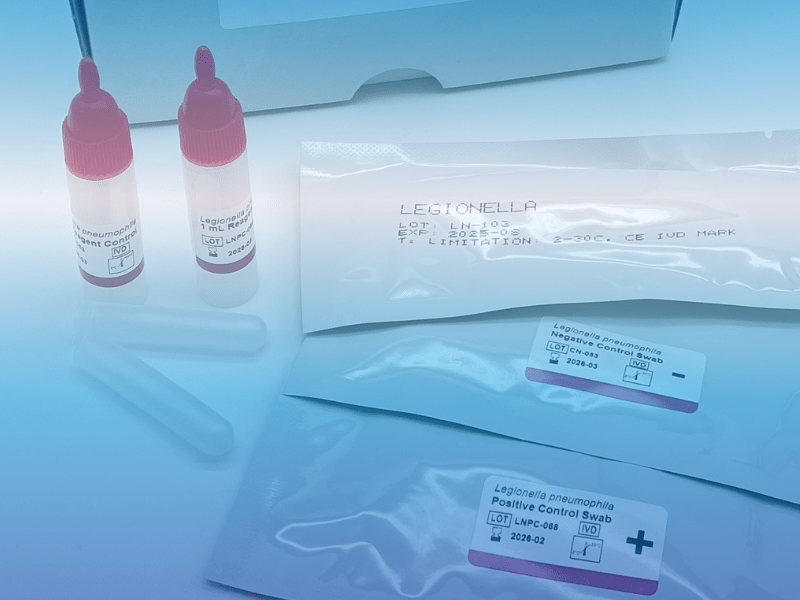
The most common method of diagnosis is the detection of the Legionella antigen using antibody-based tests (ELISA, enzyme-linked immunosorbent assay). Antigen secretion can be detected after 24 hours and is present for several weeks. The urine antigen tests only detect L.pneumophila infections of serogroup 1 and are therefore suitable for community-acquired or acute travel-associated diseases. Another option is immunochromatographic rapid antigen tests.
Direct cultural detection of the pathogen from sputum or respiratory materials on special culture media is the gold standard. This test takes 3-10 days until a result is available and is regularly used to verify positive antigen detection.
The PCR method is used for the direct pathogen detection of Legionella genes from sputum or respiratory materials. In urine, however, the PCR method is unsuitable as there are no large DNA target molecules in urine samples.
Serological detection of antibodies against Legionella in serum (IgG, IgM) is carried out using enzyme-linked immunosorbent assay (ELISA) or the immunofluorescence method. Serological antibody detection is not useful for diagnosing an acute infection, as serum antibodies are only formed in the 6th-8th week of illness and are difficult to interpret [5].
Obligation to report
The detection of L.pneumophila has been subject to mandatory reporting since 2001 by §§ 7, 8, 9 of the Infection Protection Act (IfSG). The disease should be reported to the responsible public health department no later than 24 hours after the laboratory becomes aware [4].
On the RKI website you will find documents from investigations of legionellosis cases and outbreaks, as well as documents for health authorities.
Legionella: Performance data and comparison of diagnostic tests on the market
For antigen detection in urine, morning urine is preferred. 5-10mL of the middle urine portion (after 2-3 seconds) is taken. For testing with the Rapid-VIDITEST, the sample can be stored at room temperature for 24 hours or at +2 to +8°C for up to 14 days. The test is quick and easy to perform. Four drops of the urine sample are placed on the marked window of the test cassette and after a reaction time of 15 minutes, the result can be read immediately.
For the testing of L. pneumophila by antigen detection, there are currently several rapid test options on the diagnostic market that detect serogroup 1. Most rapid tests are of immunochromatographic format. The implementation of the ELISA method requires a microtiter plate and an incubator. Therefore, this alternative proves to be very time-consuming until a result is available.
The immunochromatographic rapid test VIDITEST has various advantages, such as a simple and fast pre-analysis and reliable results. A comparison of the performance data of several commercially available rapid diagnostic tests shows that the performance characteristics of the Rapid-VIDITEST are the best. After all, the Rapid-VIDITEST has a sensitivity and specificity of more than 99%.
The kit has an external positive and negative control. With the Rapid-VIDITEST, antigen secretion can be successfully detected after just 3 days and the result is available after a few minutes. This rapid test can be sent without refrigeration.
Rapid antigen tests are primarily used to detect possible diseases. A reliable test that is quick and easy to use enables a correct diagnosis [6].
EMB code number and GOÄ
Billing code according to EMB: 32707-Bacteriological tests: Antigen immunoassay/immunofluorescence.
GOÄ: number 250, fee 14,57eur-Detection of bacterial antigens, ligand assay, per examination [7].
Advantages of the Point of Care Legionella rapid test for medical facilities:
- Result within 15 minutes
- Sensitivity and specificity > 99%
- Simple handling
- Antigen detection using urine
- Includes external positive and negative control
- Detection of antigen excretion after just 3 days
For further information on the product or the price, please contact us by email or telephone.
- Jain, H. Sulaiman, SA. Pokhrel, P. Khan, NU. Verma, A. (2023).Unveiling the recent outbreak of Legionella in Poland: approaches and obstacles – an editorial. Ann Med Surg (Lond). Oct 20;85(12):5855-5858. doi: 10.1097/MS9.0000000000001434. PMID: 38098596; PMCID: PMC10718324.
- Wuppertal: 13 Krankheitsfälle durch Legionellen. (2023). Check Natura. URL: https://checknatura.de/Aktuelles/2023/August-2023/Legionellen-in-Wuppertal/
- Epidemiologisches Bulletin. (2023). Robert Koch Institut
- Dupke, S. Buchholz, U. Fastner, J. Förster, C. Frank, C. Lewin, A. Rickerts, V. Selinka, HC. (2023). Auswirkungen des Klimawandels auf wasserbürtige Infektionen und Intoxikationen. Journal of Health Monitoring.
- Legionellose. (2019). Robert Koch Institut. RKI-Ratgeber
- One step Legionella Card test for the detection of Legionella pneumophila from urine specimen. (2019). Instruction manual. VIDIA
- Gebührenordnung für Ärzte. (2013). Verband der privaten Krankenversicherung e.V